Team:Missouri Miners/Glucose Sensor
From 2011.igem.org
(Fixed formatting issues, put in hyper links) |
Lordcheeto (Talk | contribs) |
||
| Line 1: | Line 1: | ||
{{OrganizationS&T}} | {{OrganizationS&T}} | ||
| - | <div id="box" style="position: relative; width: 740px; margin-left: 30px; top:-20px; padding: 5px; background-color: #000000;"> | + | <!--<div id="box" style="position: relative; width: 740px; margin-left: 30px; top:-20px; padding: 5px; background-color: #000000;"> |
| - | <div id="template" style="font-weight: regular; font-size: medium; color: silver; padding: 5px;"> | + | <div id="template" style="font-weight: regular; font-size: medium; color: silver; padding: 5px;">--> |
| - | <h1>Glucose Sensors </h1><br /> | + | <div style="width: 740px; margin: 0px 30px; padding: 5px; background-color: #000000;"> |
| - | + | <h1>Glucose Sensors</h1> | |
| - | + | <br /> | |
| - | Type one diabetes is characterized by the body’s inability to produce insulin and is caused by the death or malfunction of the | + | <h3>Background</h3> |
| - | Insulin is produced in the Islets of Langerhans (a section of the pancreas) where glucose in the blood is detected. | + | <p>Type one diabetes is characterized by the body’s inability to produce insulin and is caused by the death or malfunction of the ß-cells in the pancreas. Insulin is the hormone that decreases the blood glucose concentration by inducing the cellular intake of glucose.</p> |
| - | + | <p>Insulin is produced in the Islets of Langerhans (a section of the pancreas) where glucose in the blood is detected. ß-cells in this region produce insulin by monitoring the ratio of ATP (adenosine triphosphate) versus ADP (adenosine diphosphate). When the ATP level is increased the K+ channels close, creating an increase of Ca+ ions in the cell. The unbalance of ions signals the golgi complex to secrete insulin. If the ß-cells die or malfunction then insulin cannot be produced. (http://www.abcam.com/index.html?pageconfig=resource&rid=10602&pid=7) </p> | |
| - | + | <br /> | |
| - | [[File:Insulin_production_model.jpg]] | + | <div style="text-align:center"> |
| - | + | [[File:Insulin_production_model.jpg]] | |
| - | + | </div> | |
| - | In the United States alone, it is estimated that 3 million people are affected by type one diabetes. Complications that arise due to this disease include heart disease, stroke, high blood pressure, blindness, kidney disease, and neuropathy. The American Diabetes Association has estimated that diabetes costs America over $200 billion per year in diagnosis and treatment | + | <br /> |
| - | + | <h3>Project Justification</h3> | |
| - | Project Inspiration< | + | <p>In the United States alone, it is estimated that 3 million people are affected by type one diabetes. Complications that arise due to this disease include heart disease, stroke, high blood pressure, blindness, kidney disease, and neuropathy. The American Diabetes Association has estimated that diabetes costs America over $200 billion per year in diagnosis and treatment (http://www.diabetes.org ).</p> |
| - | + | <br /> | |
| - | Unfortunately, biobricks for this complete system were not entered into the registry. Our team decided to continue their work so these biobricks could be available on the registry. In addition to submitting this part to the registry our team wanted to modify the part so that is was sensitive to glucose at multiple concentrations. By doing this, we could use the biobrick to develop an economical glucose sensor.< | + | <h3>Project Inspiration</h3> |
| - | + | <p>Our group was brainstorming project ideas one day when a team member spoke up and announced that he has been afflicted with type one diabetes since he was a child. He asked the group if synthetic biology could be used to help people like him with this disease. Research into the topic soon revealed that, in 2007, the Taipei iGEM team had already come up with an answer (http://parts.mit.edu/igem07/index.php/Taipei). They had designed a system with a glucose sensitive promoter and a eYFP reporter gene. This gene could be substituted for an insulin production gene, so that when glucose is present in the environment, insulin is produced. This system has applications in insulin pump technologies.</p> | |
| - | Project Goal< | + | <p>Unfortunately, biobricks for this complete system were not entered into the registry. Our team decided to continue their work so these biobricks could be available on the registry. In addition to submitting this part to the registry our team wanted to modify the part so that is was sensitive to glucose at multiple concentrations. By doing this, we could use the biobrick to develop an economical glucose sensor.</p> |
| - | Our goal is to model a system that can measure glucose levels and produce insulin as needed. In the future, this system could lead to cheaper blood glucose testing devices or a economic and efficient insulin pump. To achieve this goal we are utilizing the EnvZ-OmpR signal transduction pathway. This pathway is endogenous to E.Coli and has been well characterized. EnvZ is a osmolarity sensor on the inner membrane of E.Coli. When glucose is added to the environment it induces a change in osmolarity and activates EnvZ. EnvZ then phosphorylates the OmpR transcription factor. When OmpR is phosphorylated it binds to the OmpR promoter and recruits RNA polymerase to begin downstream transcription. | + | <br /> |
| - | + | <h3>Project Goal</h3> | |
| - | </ | + | <p>Our goal is to model a system that can measure glucose levels and produce insulin as needed. In the future, this system could lead to cheaper blood glucose testing devices or a economic and efficient insulin pump. To achieve this goal we are utilizing the EnvZ-OmpR signal transduction pathway. This pathway is endogenous to E.Coli and has been well characterized. EnvZ is a osmolarity sensor on the inner membrane of E.Coli. When glucose is added to the environment it induces a change in osmolarity and activates EnvZ. EnvZ then phosphorylates the OmpR transcription factor. When OmpR is phosphorylated it binds to the OmpR promoter and recruits RNA polymerase to begin downstream transcription.</p> |
</div> | </div> | ||
Revision as of 05:44, 27 September 2011
Glucose Sensors
Background
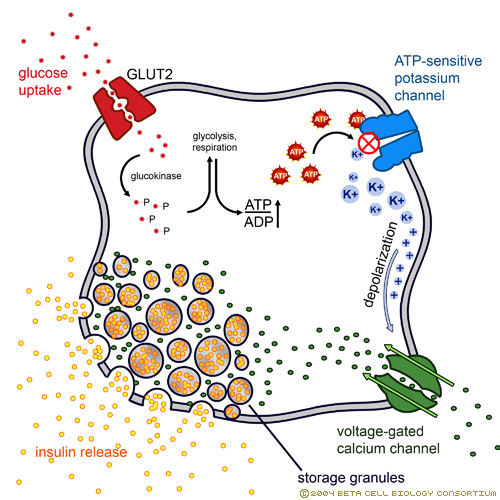
Type one diabetes is characterized by the body’s inability to produce insulin and is caused by the death or malfunction of the ß-cells in the pancreas. Insulin is the hormone that decreases the blood glucose concentration by inducing the cellular intake of glucose.
Insulin is produced in the Islets of Langerhans (a section of the pancreas) where glucose in the blood is detected. ß-cells in this region produce insulin by monitoring the ratio of ATP (adenosine triphosphate) versus ADP (adenosine diphosphate). When the ATP level is increased the K+ channels close, creating an increase of Ca+ ions in the cell. The unbalance of ions signals the golgi complex to secrete insulin. If the ß-cells die or malfunction then insulin cannot be produced. (http://www.abcam.com/index.html?pageconfig=resource&rid=10602&pid=7)
Project Justification
In the United States alone, it is estimated that 3 million people are affected by type one diabetes. Complications that arise due to this disease include heart disease, stroke, high blood pressure, blindness, kidney disease, and neuropathy. The American Diabetes Association has estimated that diabetes costs America over $200 billion per year in diagnosis and treatment (http://www.diabetes.org ).
Project Inspiration
Our group was brainstorming project ideas one day when a team member spoke up and announced that he has been afflicted with type one diabetes since he was a child. He asked the group if synthetic biology could be used to help people like him with this disease. Research into the topic soon revealed that, in 2007, the Taipei iGEM team had already come up with an answer (http://parts.mit.edu/igem07/index.php/Taipei). They had designed a system with a glucose sensitive promoter and a eYFP reporter gene. This gene could be substituted for an insulin production gene, so that when glucose is present in the environment, insulin is produced. This system has applications in insulin pump technologies.
Unfortunately, biobricks for this complete system were not entered into the registry. Our team decided to continue their work so these biobricks could be available on the registry. In addition to submitting this part to the registry our team wanted to modify the part so that is was sensitive to glucose at multiple concentrations. By doing this, we could use the biobrick to develop an economical glucose sensor.
Project Goal
Our goal is to model a system that can measure glucose levels and produce insulin as needed. In the future, this system could lead to cheaper blood glucose testing devices or a economic and efficient insulin pump. To achieve this goal we are utilizing the EnvZ-OmpR signal transduction pathway. This pathway is endogenous to E.Coli and has been well characterized. EnvZ is a osmolarity sensor on the inner membrane of E.Coli. When glucose is added to the environment it induces a change in osmolarity and activates EnvZ. EnvZ then phosphorylates the OmpR transcription factor. When OmpR is phosphorylated it binds to the OmpR promoter and recruits RNA polymerase to begin downstream transcription.
 "
"